Identifying the business/technology issues and solutions for making clinical genomics standard of care – with a call to action

Genomics as standard of care - The top 15 issues and barriers slowing clinical adoption
- Share this post:
Introduction
Clinical genomics has the potential to revolutionize healthcare by providing personalized treatment options based on a patient’s unique genetic makeup. However, despite its promise, the adoption of clinical genomics as standard of care has been slow. In this blog post, we will examine the major issues affecting clinical adoption and discuss what needs to happen next.
The ever-present barrier to the adoption of clinical genomics is all the competing system priorities that require funding and resources. Additionally, the Meaningful Use program by the U.S. federal government, which started in 2011, forced most IT budgets to focus on regulatory compliance rather than advancing strategic programs like genomics.
Another continuing issue is that genetic testing and related services are often doctor or specialty-centered rather than patient-centered. This lack of a system-wide plan can lead to a lack of standardization and inconsistent results. Building a comprehensive clinical genomics program is a highly complex activity.
My list of issues and barriers
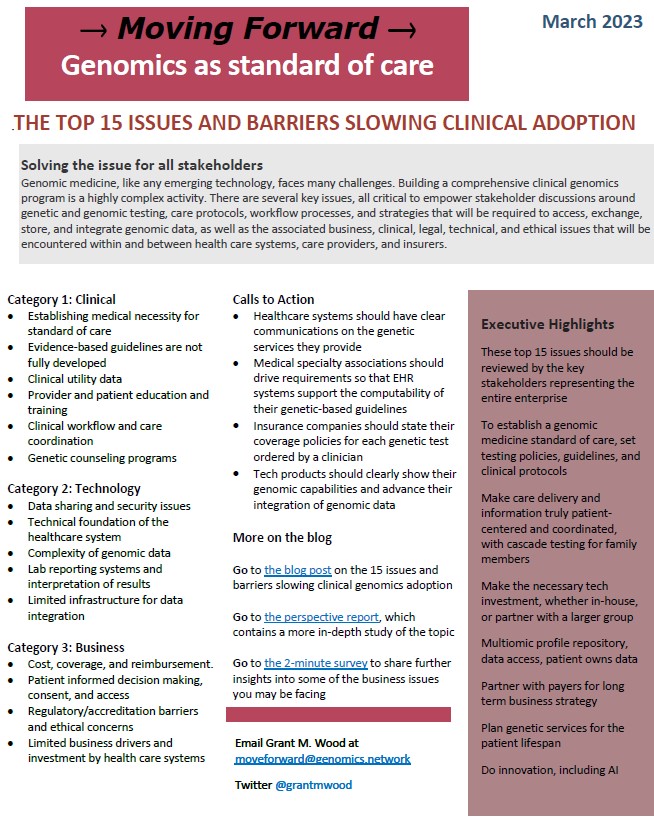
Based on my knowledge, experience, and industry involvement, I have compiled a list of 15 issues and barriers that should be systematically reviewed, followed by real efforts to solve each, starting with the clinical genomics champions and motivated stakeholders across the entire enterprise. Of course, there are more than 15 issues to work on, but I recommend starting with these significant topics first.
- Establishing medical necessity. What are the risks and benefits of genomic testing? What policies for test ordering and clinical protocols need to be formalized? These and other related questions must be reviewed before the healthcare system begins its journey toward initiating genomics as standard of care.
- Evidence-based clinical guidelines are not fully developed or easily implemented. There are limited guidelines for how to interpret and use genetic and genomic information in clinical decision-making. While some clinical guidelines are well-established, the broad scope and quality of these guidelines can vary depending on the medical condition being treated.
- Clinical utility data. Clinical utility data provides insight into how well a test performs in clinical settings and how it compares with diagnostic tests developed at competing labs. This data allows medical economists to determine the cost-effectiveness of different genomic tests by calculating their return on investment (ROI).
- Provider and patient education and training. Some healthcare providers still do not have the complete knowledge and training to interpret and use genomic information in clinical decision-making. Patients must also be educated on their responsibility and how genetics fits into their care.
- Clinical workflow. The consequence of genomics on clinical workflow is a critical component of the whole plan. If clinicians are already having trouble integrating basic clinical data into their daily practice, it will be crucial to figure out how genomic-based care coordination can help without completely overwhelming the individual clinical provider, and by extension, the whole care team.
- Genetic counseling programs. Gene counselors are essential to supporting physicians in delivering optimized genomics-based care. Healthcare systems still underpay them, so many counselors go outside of healthcare delivery and into industry. Another missing piece of this issue is how most medical organizations lack an enterprise-wide family health history program that focuses on a patient’s risk for genetic disorders.
- Cost, coverage, and reimbursement. Genomic testing costs have decreased substantially, but insurance companies still have different policies for coverage and reimbursement. Too often this gets in the way of decision-making about how best to diagnose and treat the patient. A streamlined test selection, pre-authorization, and test ordering process is required to solve this problem. (See Call-to-Action #3).
- Data sharing and security issues. Genomic data uses the same security technologies that are used for the general patient record, but computer systems that will store genomic data for a lifetime require policies covering privacy, confidentiality, and data ownership. The accessibility and sharing of genomic data need a smart design, and also require providers, patients, and health IT to work together.
- Technical foundation. Hardware, software, lab data interfaces, EHR interoperability, genomic data quality, data management and governance, analysis, visualization, and the technical talent to manage it all, are required technical requirements. The healthcare system should build a capacity for digital innovation and not just system maintenance.
- Complexity of genomic data. Management of genomic data is complicated and requires specialized expertise to interpret and use in clinical decision-making. A genomic data repository should be built with the ability to query any chromosome or gene down to the level of single nucleotide polymorphism (SNP). The repository should contain the patient’s whole genome, and not just the much smaller variant call file (VCF).
- Lab reporting systems and interpretation of results. The lack of a coding system to identify unique tests makes it difficult to compare results across similar assays (see the featured post Adopting one ID for every uniquely offered genetic test). There is also an absence of a standardized approach for interpreting test result data for clinical decision-making. Third-party vendors offer more comprehensive interpretation tools, but EHRs should become far more integrated and intuitive for the clinician than they are today.
- Limited infrastructure for data integration. There is a lack of technical infrastructure in place to support the integration of genomic data into standard patient care, including full system interoperability through the adoption of available data standards. Non-proprietary data interfaces are needed to enable genomic data to be transmitted from laboratories to EHRs and/or genomic repositories, and also between the various computer applications that make up the future clinical genomics ecosystem.
- Patient-informed decision-making, consent, and access. Patients should be informed about the risks and benefits of genetic and genomic testing. A patient testing and data-sharing consent application should be developed. This would allow them to manage data consenting situations, along with directing information access to themselves, healthcare providers, researchers, and any other entity of the patient’s choice.
- Regulatory/accreditation barriers and ethical concerns. Regulation of genetic tests adds extra time and expense to the development and marketing of new genetic tests. Different countries have different regulations for genetic testing, which can make it difficult for companies to market their clinical genomic services internationally. Ethical concerns may include using patient-generated data and data from direct-to-consumer services.
- Limited business drivers and investment by healthcare systems. Clinical genomics, if properly designed and implemented, can generate new revenue streams and provide a competitive advantage. Healthcare delivery systems that have a clinical genomics program are seen as more advanced and innovative. But most system websites do not even list a full menu of clinical genomic services. (See Call-to-Action #1).
Perspective Report
A comprehensive review of this post
Factsheet Summary
A one-page summary of the post’s major issues, including executive highlights
Survey
Business issues that may be slowing the full implementation of clinical genomics
The Call to Action
- Healthcare systems should have clear communications on the genetic services they provide. (CTA#1)
- Medical specialty associations should drive requirements so that EHR systems support the computability of their genetic-based guidelines. (CTA#2)
- Insurance companies should state their coverage policies for each genetic test ordered by a clinician. (CTA#3)
Tech products should clearly show their genomic capabilities and advance their integration of genomic data. (CTA#4)
We really want to see these actions come to life. Your input and ideas will determine the next steps and development of each action strategy. Progress will be tracked in future posts. This blog is not designed for passive readers. If you agree with these actions, let’s work together to make it happen. We will pursue these and future Call-to-Actions over time until we can verify that they have been achieved. Stay tuned!
Take a quick 2-minute survey
To gather further insights into some of the business issues you may be facing, take this fast and easy survey. We will use the results in a follow-up post and continuing discussion of this topic.
Conclusion
Clinical genomics has the potential to revolutionize healthcare, but there are several issues and barriers that are slowing its adoption. To overcome these barriers, there needs to be a concerted effort by all stakeholders to address the clinical, business, technology, and governance issues. When we as an industry address and solve the issues on this list, we can move forward and make clinical genomics the standard of care.