Identifying the business/technology issues and solutions for making clinical genomics standard of care – with a call to action

Patient-centered genomics-based care requires real
genomics-based care coordination
- Share this post:
Introduction
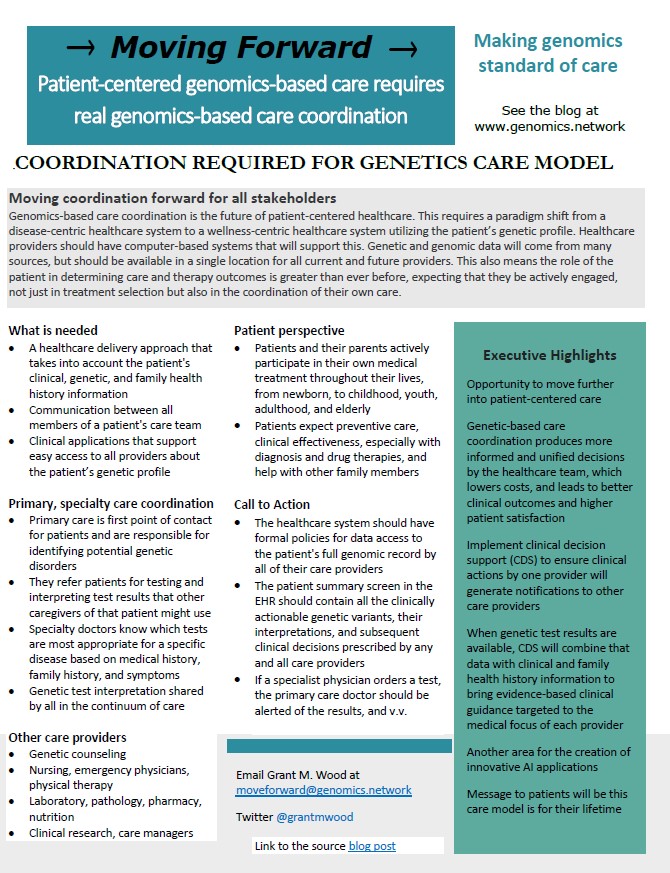
The integration of genomics into patient care is complex and requires coordination between various medical practitioners. This goal is contingent on high-quality data that is easily accessible and applicable in the patient care setting. Despite advancements in electronic health record (EHR) systems, work remains to be done to optimize their ability to support genomically informed care. EHR systems used by the care team should access the patient’s genomic data repository, store genetic and genomic test result data, and utilize clinical decision support functionality to review the most effective treatment options.
What is Needed
Patient-centered care is a healthcare delivery approach that focuses on the needs, preferences, and values of the individual patient. Genetic-based patient-centered care takes into account the patient’s clinical, genetic, and family health history information and uses it to inform the development of personalized health plans, determining the most appropriate diagnostic tests, treatments, and preventive measures. It involves coordinating the molecular knowledge of the patient to ensure that multiple treatment plans from multiple care providers work as one, with no duplications or gaps in the patient’s care. Current medical record system designs do not support this, so technology may need to be rethought and redesigned to achieve true patient-centered genetic-based healthcare.
My Experience
Healthcare systems still lack patient-facing websites that describe genetic-based services and how the information would be coordinated among current and future care providers. Test results are not received as discrete and computable data in the EHR, and specialist results are not known to primary care. Duplicate genetic tests are ordered 3-5% of the time, and patients still do not have access to their test results and data. It is true, however, that some gaps are being filled by integrated third-party solutions in EHRs.
Genetic and genomic data comes from several sources
Depending on the service provided and the expertise of the healthcare practitioner in charge, multiple and diverse clinical scenarios generate genetic data with varying degrees of complexity. Genetic and genomic data will come from several sources that need to be coordinated.
Primary Care Physicians
Primary care doctors are the first point of contact for patients and are responsible for identifying potential genetic disorders, referring patients for genetic testing, and interpreting test results. They must stay up to date with advances in genetic-based care and be familiar with available resources and support systems. Additionally, they must collaborate with specialty providers and maintain a lifetime patient medical record to ensure comprehensive and integrated care. Coordinated care means everyone is responsible for helping patients navigate the complex healthcare system to access the resources they need to manage their condition effectively.
Specialty Physicians
Specialty doctors play a key role in coordinating genetic-based care, providing expert medical care to patients with specific conditions. They must work closely with primary care doctors, genetic counselors, and other healthcare professionals to ensure that all relevant information is shared and that a comprehensive care plan is seamlessly administered. They will use germline testing for risk assessment, diagnosis, treatment guidance, and somatic testing to optimize therapeutic choice. Specialty doctors must also keep up with advances in genetic testing and treatment options, be knowledgeable about the latest developments in their field and be able to incorporate new information into their patient care plans.
Genetic Counselors
The need for genetic counselors is increasing as routine genetic and genomic testing, data analysis, and clinical interpretation become the norm in healthcare. Counselors collect and analyze a family medical history to determine risk and propose appropriate tests. They coordinate the ordering of tests and discuss the lab results with the patient and the doctor. They also provide information, assist with decision-making, and facilitate other processes related to patient management and follow-up. An integrated data system and provider-specific decision support are needed for the effective management of this process.
Perspective Report
A comprehensive review of this post
Factsheet Summary
A one-page summary of the post’s major issues, including executive highlights
Two Minute Survey
The survey questions will investigate various areas where genetics-based care coordination may or may not be operating well.
The Call to Action
Does your local healthcare system on its website clearly list all the genetic and genomic services they provide and how to access them? Here are three other major we can do together –
- Does the healthcare system have formal policies for data access to the patient’s full genomic record by all of their care providers?
- Does the patient summary screen in the EHR should contain all the clinically actionable genetic variants, their interpretations, and subsequent clinical decisions prescribed by any and all providers?
- If a specialist physician orders a test, is the primary care doctor alerted of the results, and vice versa?
To participate in this effort, join us at Call-to-Action #6.
My idea is to create a content example to show them why this information is important to their patients. I would like to get volunteers who want to try this with their local healthcare organizations.
The expanded team of healthcare providers who will access the data in the continuum of care
Tertiary and ancillary providers play an important role in genetics-based care, providing ongoing support and care to help patients manage their condition. Laboratory and pathology conduct cytogenetic and molecular testing, and contribute to variant databases. Pharmacogenomic testing can inform individualized treatment plans for patients with drug therapies. Pharmacists actively promote and take part in studies, collaborative efforts, and networks to help integrate pharmacogenomics into clinical practice. Diseases that run in families can be devastating and even fatal over time. For hospitalists and emergency care, some of these conditions may cause emergency visits or long stays in the hospital
Nurses play a critical role in coordinating genetic-based care as they assist patients and families in navigating the complex healthcare system related to genetic conditions. They work closely with clinicians to ensure that patients complete tests and treatments in a timely and effective manner. They also provide resources and referrals for patients and families, as well as follow-up care that is centered on the patient. Evidence suggests that hereditary factors play a role in the development of many of the dysmorphic disorders that physical therapists treat in clinical practice. Nutritional genomics can help identify personalized dietary interventions based on an individual’s genetic makeup, inform healthcare providers about how certain nutrients interact with medications, and accelerate the search for treatments. Doctors and patients must work together with clinical research to accelerate the search for treatments. Care managers must evaluate the validity and utility of clinical genetic and genomic testing to make educated decisions about how much to pay for medical services.

Genetic-Based Care Coordination From the Patient and Family Perspective
Care coordination is the deliberate organization of a patient’s care activities between two or more providers, with the goal of getting better care. If implemented correctly, it should reduce the risk of medical errors, duplicative tests and treatments, and adverse drug interactions. It also helps to reduce the burden on patients, who are often overwhelmed by the demands of managing their care and what the costs might be. Cost-benefit analysis is especially important when it comes to genetic services, where testing and interpretation could be expensive but results can provide knowledge that helps the patient and their loved ones for their lifetime. Healthcare providers must understand the lifestyle needs and socio-economic realities of patients to make informed treatment choices.
Genetic-based healthcare has the potential to greatly benefit families by providing them with a deeper understanding of their health risks and inheritance patterns. After one family member is found to have a clinically important heritable variant, family care coordination should make it possible for other family members to get cascade testing. All new test results should loop back into the information about the family.
From the Perspective of the Patient Lifespan
Care coordination services must be improved and made more permanent for individuals with genetic diseases to get the care they need, as their physical, psychological, and social demands vary over their lifetime.
Prenatal and newborn
Genetic-based healthcare provides families with the opportunity to make informed reproductive decisions. It also helps diagnose genetic conditions in newborns and provides families with the necessary information to plan for their child’s future care. Risk factors such as the mother’s age, race, illnesses in siblings and other family members, and problems or loss of a previous pregnancy are used to decide which tests should be done during pregnancy to look for genetic conditions. When a genetic issue is suspected and confirmed in a newborn, it is important to coordinate care so that the infant receives treatment and the family has access to resources as the child moves through critical developmental stages.
Childhood and adolescence
The symptoms of some genetic disorders, such as those that affect intelligence and social skills, may first appear during childhood and can trigger intense and emotionally painful involvement with the healthcare system. Adolescents typically require genetic services for the early detection of disorders such as hypertrophic cardiomyopathy and long-QT syndrome, as well as other well-known disorders such as diabetes, asthma, childhood cancers, cystic fibrosis, and muscular dystrophy. Teenagers with genetic diseases may find it hard to switch from child health care to adult care and may need help making the adjustment from living at home with their parents.
Young adult to elderly years
Genetic services are used to help young adults plan a family, screen for carrier status, and identify the genomic basis of cancer and other illnesses. Pharmacogenomic testing can help choose the best drug and dose for a person, and risk can be discovered through family history. As people enter their later years, they are more likely to start making use of healthcare services. Elderly patients’ families and caregivers need assistance to meet their needs, especially if a long life is in the genes.
Conclusion – Opportunities for Moving Forward
Genetic-based care coordination has the potential to revolutionize the way we approach health care for individuals with genetic disorders. It requires coordination between various healthcare providers and technology, leading to improved patient outcomes. To reach its full potential, genetic information needs to be better integrated into electronic health records, standard protocols for sharing genetic information need to be made, and healthcare providers need to be trained in how to understand and use genetic information in patient care. Working together, healthcare providers, including physicians, nurses, counselors, therapists, labs and pharmacy, patients, researchers, and case managers, can overcome these challenges and pave the way for a future where genetic information is routinely used to optimize the care of individuals and families.
Contact Grant at moveforward@genomics.network.